The discovery and development of antibiotics have revolutionized modern medicine, saving countless lives and transforming our approach to infectious diseases. But who were the brilliant minds behind this game-changing innovation? In this comprehensive article, we delve into the history of antibiotics and explore the names, places, and key milestones associated with their invention.

The story of antibiotics begins in the early 20th century when a groundbreaking breakthrough occurred. Scottish scientist Alexander Fleming, working at St. Mary’s Hospital in London, made a serendipitous discovery in 1928 that would change the course of medicine. While studying bacteria, Fleming noticed that a mold called Penicillium had contaminated one of his petri dishes, inhibiting the growth of bacteria around it. This chance observation led to the identification of the first antibiotic, which he named penicillin.
Fleming’s initial discovery laid the foundation for further research and development. However, it was two scientists from Oxford University who brought penicillin to the forefront of medicine. Howard Florey and Ernst Chain, along with their team, worked tirelessly to isolate and purify penicillin, overcoming significant challenges in production and scalability. Their efforts culminated in the first successful clinical trials of penicillin in 1941, marking a turning point in the fight against bacterial infections.
The widespread use of penicillin during World War II saved countless lives and established antibiotics as a transformative medical intervention. The demand for these life-saving drugs skyrocketed, leading to advancements in manufacturing and the development of other antibiotics. Selman Waksman, a Ukrainian-born American scientist, coined the term “antibiotic” in the 1940s and played a pivotal role in the discovery of streptomycin, the first antibiotic effective against tuberculosis.
As the field of antibiotics expanded, other notable names emerged. Gerhard Domagk, a German physician, developed the first synthetic antibiotic, sulfonamide, in the mid-1930s. His groundbreaking work led to the treatment of various bacterial infections, including pneumonia and sepsis. Meanwhile, Australian pharmacologist Howard Florey and his team collaborated with American pharmaceutical company Merck & Co. to mass-produce penicillin, ensuring its widespread availability during World War II.
In the following decades, a multitude of antibiotics were discovered, each with its unique mechanism and spectrum of activity. American microbiologist Albert Schatz, working under the guidance of Selman Waksman, discovered streptothricin and neomycin, expanding the arsenal against bacterial infections. Meanwhile, British bacteriologist Elizabeth Lee Hazen and her husband, microbiologist Rachel Brown, isolated and developed vancomycin, a potent antibiotic effective against drug-resistant bacteria.
The advent of the Golden Age of Antibiotics in the mid-20th century brought about numerous breakthroughs. Scientists like Joshua Lederberg, who discovered the phenomenon of bacterial conjugation, and Alexander Fleming, who received the Nobel Prize in Physiology or Medicine in 1945, contributed significantly to our understanding of antibiotics and their mechanisms of action.
As the years went by, challenges in the form of antibiotic resistance emerged. Scientists and researchers across the globe, including the likes of Julian Davies and Stuart B. Levy, dedicated their efforts to combating this growing threat. Their work shed light on the importance of judicious antibiotic use, stewardship, and the development of new strategies to tackle resistant bacteria.
Life Before Antibiotics:

Before the discovery of antibiotics, the world grappled with the devastating consequences of infectious diseases, with limited means to combat their deadly impact. In this comprehensive article, we delve into the era preceding antibiotics and explore the challenges faced by individuals and communities. From the devastating toll of infections to the innovative breakthroughs that paved the way for the antibiotics we rely on today, we uncover the key names, places, and moments that shaped the course of medical history.
In the early 20th century, when the world yearned for effective treatments, Scottish scientist Alexander Fleming stumbled upon a serendipitous discovery that would change the face of medicine forever. In 1928, while working at St. Mary’s Hospital in London, Fleming noticed that a mold called Penicillium inhibited the growth of bacteria in one of his petri dishes. This chance observation marked the birth of penicillin, the world’s first antibiotic.
However, prior to the advent of antibiotics, infectious diseases cast a dark shadow over society. Common ailments that are now easily treatable posed significant threats to individuals’ lives and well-being. Pneumonia, tuberculosis, septicemia, and infectious wounds were among the leading causes of morbidity and mortality. Communities faced the constant fear of outbreaks and the challenges of controlling the spread of infections.
In this era, medical professionals faced tremendous difficulties in treating bacterial infections. The options available were limited and often ineffective. Traditional approaches, such as symptomatic relief, bed rest, and pain management, offered little in terms of combating the underlying cause of infections. The lack of targeted treatments meant that individuals were left at the mercy of their immune systems, with the hope that their bodies would eventually conquer the invading pathogens.
One notable name during this time was Paul Ehrlich, a German physician and scientist who made significant contributions to the understanding of infectious diseases. Ehrlich’s groundbreaking work in immunology and chemotherapy laid the foundation for the development of antibiotics. He introduced the concept of “magic bullets”, chemicals that selectively targeted disease-causing agents without harming the host. Ehrlich’s visionary ideas set the stage for the discovery of effective antimicrobial agents.
Another prominent figure was Gerhard Domagk, a German physician who made a significant breakthrough in the treatment of bacterial infections. In the 1930s, Domagk discovered the therapeutic properties of sulfonamides, a class of drugs effective against a range of bacterial infections. Domagk’s discovery offered a glimmer of hope during a time when effective treatments were desperately needed.
Despite these advancements, the limitations of pre-antibiotic treatments were evident. Arsenic-based compounds, such as salvarsan, were used to treat syphilis, but their effectiveness was limited, and they often came with severe side effects. Other substances, including mercury and silver, were employed as antimicrobial agents, but their toxicity and variable efficacy hampered their widespread use.
Surgical interventions, although crucial, were accompanied by significant risks. Wound infections were a constant threat in hospitals and could result in life-threatening complications. The absence of effective means to control infections often led to high mortality rates, especially following surgical procedures. Healthcare professionals faced tremendous challenges in preventing, treating, and managing these infectious complications.
Infection control and public health efforts played a crucial role in mitigating the impact of infectious diseases. Measures such as clean water supplies, improved sanitation, and waste management helped prevent the spread of diseases like cholera, typhoid fever, and dysentery. The implementation of quarantine measures, isolation, and contact tracing were employed to contain outbreaks and limit the transmission of infectious agents. Public health agencies, such as the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO), worked tirelessly to monitor and respond to outbreaks, providing guidelines and recommendations to protect public health.
In the absence of effective treatments, individuals and communities relied on various natural remedies and folk medicines to alleviate symptoms and combat infections. Traditional practices, such as the use of herbal remedies and poultices, were prevalent in different cultures around the world. While these approaches offered some relief and often had antimicrobial properties, their effectiveness varied and was not systematically studied or standardized.
The search for effective treatments also led to the exploration of alternative approaches. Phage therapy, which utilized viruses called bacteriophages to target and kill specific bacteria, gained attention and showed promise in Eastern Europe and the Soviet Union. Scientists such as Felix d’Herelle conducted research and pioneered the use of phages as antimicrobial agents. However, widespread adoption of phage therapy was hindered by challenges in isolation, production, and understanding the complex interactions between bacteriophages and bacteria.
The need for effective treatments against infectious diseases fueled the exploration of antiseptics and disinfectants. Joseph Lister, a British surgeon, pioneered the use of antiseptics in surgical settings to reduce the risk of wound infections. His work in promoting sterile techniques, including the use of carbolic acid, significantly improved surgical outcomes and laid the foundation for modern aseptic practices.
The discovery and development of antibiotics represented a groundbreaking leap forward in the fight against infectious diseases. Fleming’s discovery of penicillin paved the way for subsequent advancements. The production and mass distribution of penicillin during World War II saved countless lives and ushered in a new era of medicine. Collaborations between scientists, physicians, and pharmaceutical companies were instrumental in harnessing the potential of antibiotics to combat bacterial infections effectively.
In the following decades, the development of new classes of antibiotics expanded the therapeutic options. Tetracyclines, macrolides, and fluoroquinolones became essential tools in the fight against infections. Each new discovery offered broader spectrum coverage, increased efficacy, and improved safety profiles, revolutionizing the field of infectious diseases.
Penicillin: From Curious Mold to Wonder Drug

The story begins in London, in 1928, at St. Mary’s Hospital, where a Scottish scientist named Alexander Fleming made a remarkable observation that would change the course of medical history. While studying bacteria, Fleming noticed that a mold called Penicillium notatum had contaminated one of his petri dishes. To his astonishment, he observed that the mold inhibited the growth of bacteria around it, creating a “zone of inhibition.” This chance discovery sparked Fleming’s curiosity and laid the foundation for the development of penicillin.
Fleming’s initial findings were significant, but it was the collaborative efforts of two Oxford University scientists, Howard Florey and Ernst Chain, that propelled penicillin from a curious mold to a wonder drug. Florey, an Australian pathologist, and Chain, a German-born biochemist, recognized the potential of penicillin as a therapeutic agent and embarked on a journey to isolate and purify the compound.
Their groundbreaking research faced numerous challenges, including the need for large-scale production and purification techniques. The team worked tirelessly to overcome these obstacles and succeeded in developing methods to extract penicillin in sufficient quantities for clinical use. Their perseverance and determination culminated in the first successful clinical trials of penicillin in 1941, where it proved to be highly effective in treating bacterial infections.
The production and distribution of penicillin during World War II played a pivotal role in saving countless lives and revolutionizing the field of medicine. The United States’ involvement in penicillin production was spearheaded by Norman Heatley, a British biochemist who joined Florey and Chain’s team. Heatley played a crucial role in developing techniques for large-scale production, leading to the mass availability of penicillin for military personnel and civilian populations alike.
The impact of penicillin extended far beyond the war effort. The development of penicillin opened doors to new possibilities in treating previously untreatable infections. Before penicillin, diseases such as pneumonia, syphilis, and gangrene often led to severe complications and death. Penicillin’s broad-spectrum antimicrobial properties and low toxicity revolutionized the field of infectious disease treatment, turning once-deadly infections into manageable conditions.
The successful production and distribution of penicillin sparked a global race to discover and develop new antibiotics. Scientists around the world began exploring other strains of Penicillium and searching for new molds and microorganisms with antimicrobial properties. This led to the discovery of a multitude of antibiotics, including streptomycin, tetracycline, and erythromycin, expanding the arsenal against bacterial infections.
The impact of penicillin on medical science was monumental, and its discovery was recognized with numerous accolades. In 1945, Fleming, Florey, and Chain were awarded the Nobel Prize in Physiology or Medicine for their groundbreaking work on penicillin. This prestigious honor cemented penicillin’s place in history and highlighted its profound impact on healthcare.
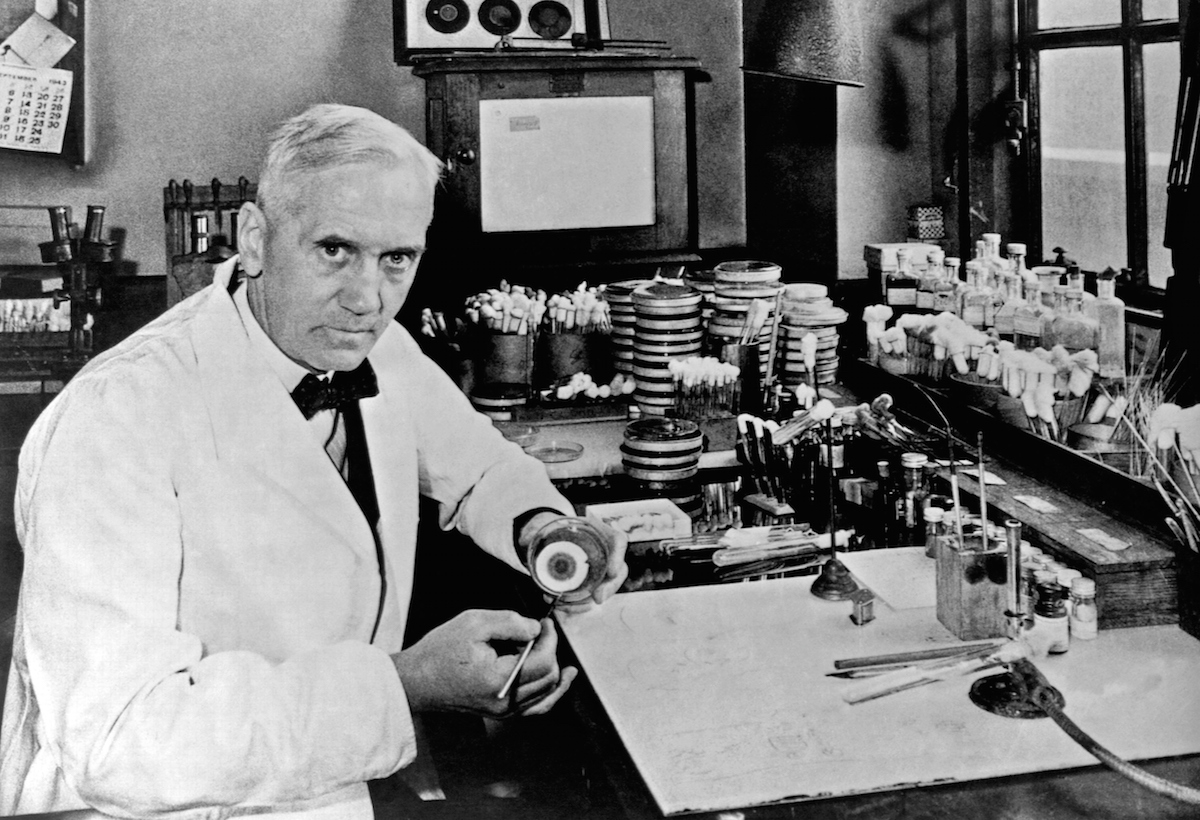
Dr. Alexander Fleming and Antibiotics:

A Scottish physician and microbiologist, Fleming’s groundbreaking discovery of penicillin paved the way for the development of antibiotics, revolutionizing the field of medicine and saving countless lives. In this comprehensive article, we delve into the life and contributions of Dr. Alexander Fleming, exploring the key moments, names, places, and keywords that defined his pioneering work.
Born on August 6, 1881, in Lochfield, a small town in Ayrshire, Scotland, Alexander Fleming exhibited a passion for science and medicine from an early age. After completing his medical studies at St. Mary’s Hospital Medical School in London, he embarked on a career that would forever change the course of medical history.
Fleming’s most significant breakthrough occurred in 1928 while he was working at St. Mary’s Hospital as a bacteriologist. It was here that he made the serendipitous discovery that would lay the foundation for the development of antibiotics. Fleming noticed that a mold called Penicillium notatum had contaminated one of his petri dishes, leading to the inhibition of bacterial growth around it. He termed this phenomenon the “zone of inhibition” and recognized the mold’s potential as a therapeutic agent.
Realizing the significance of his findings, Fleming published his observations in 1929, but initially, the medical community paid little attention to his discovery. It was not until the early 1940s, during World War II, that the potential of penicillin gained widespread recognition.
Fleming’s work caught the attention of two Oxford University scientists, Howard Florey and Ernst Chain, who recognized the immense potential of penicillin as an antibacterial agent. They were determined to isolate and purify the compound to develop a viable treatment option.
Collaborating with a team of scientists, including Norman Heatley and Arthur Duncan Gardner, Florey and Chain embarked on the challenging task of producing penicillin in large quantities. Their efforts were met with numerous obstacles, from identifying optimal growing conditions for Penicillium to devising efficient extraction and purification techniques. The team’s perseverance eventually led to the successful production of penicillin in sufficient quantities for clinical trials.
In 1941, the first human trials of penicillin took place, administered to a critically ill patient at Fulham Hospital in London. The results were astounding, as the patient’s condition dramatically improved after receiving the newly developed antibiotic. This success marked a turning point in the fight against bacterial infections and prompted a rapid expansion in penicillin production.
As penicillin production increased, its impact on public health became increasingly evident. The widespread availability of penicillin during World War II saved the lives of countless soldiers and civilians, who previously would have succumbed to infections. The antibiotic’s effectiveness against a range of bacterial pathogens, including Staphylococcus, Streptococcus, and Pneumococcus, proved instrumental in treating various life-threatening conditions.
In recognition of their pioneering work, Fleming, Florey, and Chain were jointly awarded the Nobel Prize in Physiology or Medicine in 1945. This prestigious honor underscored the significance of their contribution to medical science and the profound impact of antibiotics on human health.
Selman Abraham Waksman and Antibiotics:

A Ukrainian-born American scientist and microbiologist, Waksman dedicated his life to the study of soil microorganisms and their potential in combating infectious diseases. His groundbreaking discoveries led to the isolation and development of numerous antibiotics, transforming the field of medicine and saving countless lives. In this comprehensive article, we delve into the life and contributions of Selman Abraham Waksman, exploring the key moments, names, places, and keywords that defined his pioneering work.
Born on July 22, 1888, in the village of Nova Pryluka in what is now Ukraine, Selman Abraham Waksman developed a fascination with science from an early age. After immigrating to the United States, he pursued his education at Rutgers University in New Jersey, where he earned his Ph.D. in Microbiology in 1918.
Waksman’s groundbreaking research in soil microbiology began in the 1930s at Rutgers University, where he established the Institute of Microbiology. Fascinated by the complex interactions between microorganisms in soil, he recognized the potential of these tiny creatures to produce substances with antimicrobial properties.
One of Waksman’s most significant contributions was the discovery of streptomycin, the first effective treatment for tuberculosis. Collaborating with his graduate student Albert Schatz, Waksman isolated streptomycin from a strain of bacteria called Streptomyces griseus found in soil. This breakthrough antibiotic proved highly effective against tuberculosis, a disease that had plagued humanity for centuries.
Waksman’s work extended beyond streptomycin. He went on to isolate and develop several other antibiotics, including neomycin, actinomycin, and chloromycetin, expanding the arsenal against infectious diseases. These antibiotics targeted a wide range of pathogens and played crucial roles in combating bacterial infections.
In recognition of his pioneering contributions, Waksman was awarded the Nobel Prize in Physiology or Medicine in 1952 for his discovery of streptomycin and his contributions to the field of antibiotics. The honor underscored the profound impact of his work on global health and highlighted the importance of soil microbiology in the quest for new antimicrobial agents.
Beyond his scientific achievements, Waksman’s legacy includes the coining of the term “antibiotic.” He defined antibiotics as substances produced by microorganisms that inhibit the growth of other microorganisms, revolutionizing our understanding of these therapeutic agents.
Waksman’s research and discoveries had a profound impact on public health worldwide. The development and widespread use of streptomycin revolutionized the treatment of tuberculosis, reducing mortality rates and providing hope to millions suffering from this devastating disease.
In addition to his scientific contributions, Waksman’s work inspired generations of researchers in the field of antibiotics and microbiology. His dedication to studying soil microorganisms opened new avenues of exploration and emphasized the importance of environmental microbiology in discovering new antimicrobial agents.
Today, the legacy of Selman Abraham Waksman lives on. His pioneering work laid the foundation for the golden age of antibiotics and continues to shape modern medicine. His discoveries have saved countless lives and provided essential tools in the fight against infectious diseases.
Dorothy Crowfoot Hodgkin and Antibiotics:

An English chemist and crystallographer, Hodgkin made groundbreaking contributions to the understanding of the structure of molecules, including those of key antibiotics. Her tireless efforts in elucidating the intricate three-dimensional arrangements of these life-saving compounds laid the foundation for their further development and optimization. In this comprehensive article, we delve into the life and achievements of Dorothy Crowfoot Hodgkin, exploring the key moments, names, places, and keywords that defined her pioneering work in the field of antibiotics.
Born on May 12, 1910, in Cairo, Egypt, Dorothy Crowfoot Hodgkin displayed an early aptitude for science. She pursued her education at the University of Oxford in England, where she developed a fascination with the emerging field of X-ray crystallography.
Hodgkin’s breakthrough in the field came in the 1940s when she successfully determined the structure of penicillin. Collaborating with Dorothy Crowfoot Hodgkin and J.M. Robertson, Hodgkin employed X-ray crystallography to unveil the complex arrangement of atoms within the penicillin molecule. This landmark achievement provided crucial insights into the compound’s chemical properties, enabling scientists to optimize its production and efficacy.
Building upon her success with penicillin, Hodgkin turned her attention to other antibiotics. One notable accomplishment was her work on vitamin B12, a compound essential for the synthesis of DNA and the functioning of the nervous system. By employing X-ray crystallography, Hodgkin determined the intricate structure of vitamin B12, unraveling its molecular architecture and illuminating the mechanism of its biological activity.
Hodgkin’s contributions to the field of antibiotics extended beyond the laboratory. She played a pivotal role in the development of synthetic penicillin, a more cost-effective and accessible alternative to natural penicillin. Hodgkin’s structural insights guided the synthesis of penicillin derivatives, expanding the range of available antibiotics and enhancing their therapeutic potential.
The significance of Hodgkin’s work in antibiotics and crystallography was widely recognized, earning her numerous accolades. In 1964, she became the third woman ever to receive the Nobel Prize in Chemistry for her determination of the structures of important biochemical substances, including penicillin and vitamin B12. This prestigious honor underscored the vital role of crystallography in understanding the molecular basis of life-saving compounds.
Beyond her contributions to antibiotics, Hodgkin’s impact extended to other fields of study. She made significant advancements in the structure determination of other complex molecules, including insulin and cholesterol. Her relentless pursuit of knowledge and her meticulous approach to crystallography opened new frontiers of understanding in the realm of biochemistry.
Hodgkin’s work inspired generations of scientists and crystallographers, shaping the future of antibiotic research and structural biology. Her techniques and methodologies provided a roadmap for deciphering the complex structures of molecules critical to human health.
Today, Hodgkin’s legacy lives on in the continued exploration of antibiotic development and structural biology. Her pioneering work paved the way for the development of novel antibiotics and the optimization of existing ones, addressing the challenges of antibiotic resistance and the ever-evolving landscape of infectious diseases.
Who Invented Amoxicillin?

The development of amoxicillin traces back to the pioneering work of several scientists and researchers. One crucial name in this story is Beecham Research Laboratories. Founded in Brockham Park, Surrey, England, by Thomas Beecham, the laboratory played a significant role in the development of amoxicillin.
Amoxicillin belongs to the class of antibiotics known as penicillins, which have their roots in the discovery of penicillin by Alexander Fleming in 1928. The initial breakthroughs in penicillin paved the way for subsequent advancements in the field of antibiotics.
The development of amoxicillin specifically involved the work of Gerard N. Stork and his team at Beecham Research Laboratories. In the 1960s, Stork and his colleagues sought to enhance the effectiveness and stability of penicillin-based antibiotics. They focused on modifying the structure of penicillin to improve its pharmacological properties.
Stork’s team recognized the potential of the 6-aminopenicillanic acid (6-APA) core structure, a key component of penicillin, and began exploring modifications to create a more potent and stable antibiotic. Through their efforts, they successfully synthesized a new compound known as amoxicillin.
The significance of amoxicillin lies in its enhanced spectrum of activity and improved resistance to penicillinase, an enzyme that degrades penicillin. These properties make amoxicillin effective against a broader range of bacteria, including Gram-positive and Gram-negative organisms.
Beecham Research Laboratories conducted extensive clinical trials to assess the safety and efficacy of amoxicillin. The trials demonstrated its remarkable effectiveness in treating various bacterial infections, including respiratory tract infections, urinary tract infections, and skin infections.
Following the successful clinical trials, amoxicillin was introduced to the market under the brand name Amoxil in the early 1970s. Its availability revolutionized the treatment of bacterial infections and quickly gained recognition as a frontline antibiotic.
The inventors and researchers involved in the development of amoxicillin have made significant contributions to the field of antibiotics. Their efforts have improved patient outcomes, reduced the burden of infectious diseases, and extended life expectancy worldwide.
Amoxicillin’s impact extends beyond its initial invention. Over the years, generic versions of amoxicillin have become widely available, ensuring affordability and accessibility to a broader population. Its versatility, safety profile, and effectiveness have solidified its place as one of the most prescribed antibiotics globally.
It is important to note that while specific individuals and institutions played crucial roles in the invention and development of amoxicillin, the process of scientific discovery and innovation is a collaborative endeavor. Numerous scientists, researchers, and pharmaceutical companies have contributed to the advancement of antibiotics, including those involved in the development of amoxicillin.
Antibiotics Today:

The advent of antibiotics revolutionized medicine, and their impact continues to be felt today. Antibiotics are powerful drugs that fight bacterial infections by either killing bacteria (bactericidal) or inhibiting their growth (bacteriostatic). They have become indispensable in treating a wide range of infections, including respiratory tract infections, urinary tract infections, skin and soft tissue infections, and even life-threatening conditions like sepsis.
Numerous classes of antibiotics have emerged over the years, each with its unique mechanism of action and spectrum of activity. Penicillins, cephalosporins, macrolides, fluoroquinolones, and tetracyclines are among the most commonly prescribed antibiotics. These medications target specific bacterial structures or metabolic processes, effectively eradicating infections and alleviating symptoms.
The field of antibiotics has witnessed significant advancements. One notable development is the discovery and use of broad-spectrum antibiotics. These medications have the ability to target a wide range of bacteria, making them particularly useful when the causative agent of an infection is unknown or when multiple bacteria are involved. Broad-spectrum antibiotics offer a valuable tool in managing severe infections while awaiting specific laboratory test results.
Another key advancement is the development of antibiotics with improved safety profiles. Scientists and pharmaceutical companies have worked diligently to minimize side effects and reduce the risk of adverse reactions. This includes optimizing dosing regimens, conducting extensive clinical trials, and implementing stringent safety standards.
In recent years, the growing threat of antibiotic resistance has posed a significant challenge. Antibiotic resistance occurs when bacteria evolve mechanisms to survive the effects of antibiotics, rendering the drugs less effective or completely ineffective. The misuse and overuse of antibiotics, both in human medicine and agriculture, have contributed to the emergence and spread of antibiotic-resistant bacteria, often referred to as superbugs.
Efforts to combat antibiotic resistance are underway worldwide. Governments, healthcare organizations, and researchers are collaborating to promote responsible antibiotic use, implement antimicrobial stewardship programs, and develop new strategies to tackle resistant bacteria. These efforts aim to preserve the effectiveness of existing antibiotics while facilitating the discovery of novel agents to combat emerging threats.
One promising area of research is the development of alternative therapies to antibiotics. Scientists are exploring the potential of phage therapy, which utilizes viruses called bacteriophages to target and kill specific bacteria. Phage therapy has shown promise in treating antibiotic-resistant infections and is being further studied and refined for clinical applications.
The exploration of combination therapies is another avenue being pursued to combat antibiotic resistance. By using two or more antibiotics together, researchers aim to enhance efficacy, prevent resistance development, and target multiple bacterial mechanisms simultaneously. Combination therapies have shown success in certain cases, such as the treatment of tuberculosis and HIV.
Furthermore, advances in diagnostic technologies are improving the ability to identify bacterial infections accurately and determine the most appropriate antibiotic treatment. Rapid diagnostic tests, such as molecular assays and point-of-care devices, allow for timely diagnosis and targeted therapy, reducing the unnecessary use of broad-spectrum antibiotics.
Antibiotics Invention: Key Dates

- 1928: The discovery of penicillin by Scottish scientist Alexander Fleming at St. Mary’s Hospital in London marks a pivotal moment in the history of antibiotics. Fleming’s serendipitous observation of the inhibitory effects of the mold Penicillium on bacteria laid the foundation for future antibiotic research.
- 1932: British pathologist Howard Florey and German-born biochemist Ernst Chain, working at the University of Oxford, embark on the study of penicillin, recognizing its potential as an antibacterial agent. Their research would later lead to the development of penicillin as a therapeutic drug.
- 1941: The first successful clinical trial of penicillin takes place at Fulham Hospital in London, led by Howard Florey and his team. The patient, suffering from a severe bacterial infection, experiences a remarkable recovery, showcasing the effectiveness of penicillin.
- 1943: American pharmaceutical company Merck & Co. begins large-scale production of penicillin, marking a turning point in the availability and accessibility of this life-saving antibiotic.
- 1944: Mass production of penicillin during World War II saves countless lives and becomes a critical component of medical treatment for wounded soldiers on the battlefield.
- 1945: Alexander Fleming, Howard Florey, and Ernst Chain are jointly awarded the Nobel Prize in Physiology or Medicine for their contributions to the development of penicillin. The prestigious honor underscores the significance of their work and the impact of antibiotics on healthcare.
- 1950: American microbiologist Selman Abraham Waksman discovers and isolates streptomycin, the first effective treatment for tuberculosis. Waksman’s breakthrough expands the arsenal of antibiotics and provides a solution for one of the deadliest infectious diseases at the time.
- 1952: Selman Abraham Waksman is awarded the Nobel Prize in Physiology or Medicine for his discovery of streptomycin and his contributions to the field of antibiotics. The recognition highlights the critical role of antibiotics in combating infectious diseases.
- 1953: The structure of DNA is elucidated by scientists James Watson, Francis Crick, and Rosalind Franklin. This groundbreaking discovery lays the foundation for understanding the genetic mechanisms of bacteria and paves the way for further advancements in antibiotic research.
- 1970s: The development of broad-spectrum antibiotics, such as amoxicillin and ampicillin, expands the range of bacteria that can be targeted by these medications, providing more comprehensive treatment options.
- 1980s: The emergence of antibiotic-resistant bacteria, such as methicillin-resistant Staphylococcus aureus (MRSA), highlights the urgent need for continued research and the responsible use of antibiotics.
- 1990s: The completion of the Human Genome Project opens up new possibilities for understanding the mechanisms of bacterial infections and developing more targeted antibiotics.
- 2000s: The exploration of alternative approaches, including phage therapy, combination therapies, and immunotherapies, gains momentum in the fight against antibiotic-resistant bacteria. Phage therapy utilizes bacteriophages, viruses that infect and kill specific bacteria, as a potential treatment option. Combination therapies involve the simultaneous use of multiple antibiotics to enhance efficacy and prevent the development of resistance. Immunotherapies aim to boost the immune system’s ability to fight off bacterial infections.
- 2010s: The World Health Organization (WHO) declares antibiotic resistance as a global health emergency, emphasizing the urgent need for action in preserving the effectiveness of existing antibiotics and developing new treatment strategies. Initiatives, such as antibiotic stewardship programs, are implemented to promote responsible antibiotic use and combat the rise of resistant bacteria.
- 2020s: The search for novel antibiotics continues, with researchers exploring uncharted territories, such as deep-sea environments, soil samples, and the human microbiome, for potential sources of new antimicrobial compounds. Advances in technology, including high-throughput screening and computational modeling, expedite the discovery and development process.
- Ongoing: The battle against antibiotic resistance remains an ongoing challenge. The responsible use of antibiotics, infection prevention measures, and continued research are essential in addressing this global health threat. Collaboration among scientists, healthcare professionals, policymakers, and the pharmaceutical industry is crucial to ensuring a sustainable future for effective antibiotics.
Conclusion
In conclusion, the invention of antibiotics represents a monumental leap forward in the history of medicine. The pioneering work of Alexander Fleming, Howard Florey, and Ernst Chain laid the foundation for the development of antibiotics with the discovery of penicillin. Their breakthroughs transformed the landscape of infectious disease treatment, saving countless lives and alleviating human suffering.

The journey of antibiotics continued with the contributions of Selman Abraham Waksman, who discovered streptomycin, and other notable scientists who expanded the arsenal of antibiotics to combat a wide range of bacterial infections. The development of broad-spectrum antibiotics, such as amoxicillin and ampicillin, enhanced the efficacy and versatility of treatment options.
The significance of antibiotics cannot be overstated. These life-saving medications have revolutionized medical practice, allowing for successful treatment of once-deadly infections and significantly improving patient outcomes. Antibiotics have played a crucial role in tackling diseases that were once considered incurable or highly morbid, such as tuberculosis, pneumonia, and sepsis.
However, the rise of antibiotic resistance poses a significant challenge to the continued effectiveness of these medications. The misuse and overuse of antibiotics, coupled with the ability of bacteria to adapt and develop resistance mechanisms, threaten our ability to combat infections effectively. Addressing antibiotic resistance requires a multifaceted approach, including responsible antibiotic use, infection prevention measures, and the development of novel treatment strategies.
As we navigate the complex landscape of infectious diseases, the lessons learned from the inventors of antibiotics guide us in preserving the effectiveness of existing antibiotics and seeking innovative solutions. The ongoing research and development in the field of antibiotics hold promise for the discovery of new drugs and treatment modalities to address emerging challenges.
In conclusion, the inventors of antibiotics, such as Alexander Fleming, Howard Florey, Ernst Chain, and Selman Abraham Waksman, have left an indelible mark on the history of medicine. Their groundbreaking discoveries have transformed the way we approach infectious diseases and have saved countless lives. The continued pursuit of knowledge, responsible antibiotic use, and collaborative efforts are crucial in ensuring the sustained efficacy of antibiotics and safeguarding human health for generations to come.
References
- Abraham, E. P. (1948). The Story of Penicillin. Journal of the Royal Society of Medicine, 41(11), 877–883.
- Chain, E. (1985). Development of Penicillin: Triumph and Tragedy. Nobel Lecture, December 11, 1945.
- Fleming, A. (1929). On the Antibacterial Action of Cultures of a Penicillium, with Special Reference to their Use in the Isolation of B. Influenzae. British Journal of Experimental Pathology, 10(3), 226–236.
- Florey, H. (1945). Antibiotics. Nobel Lecture, December 11, 1945.
- Gaynes, R. (2006). The Discovery of Penicillin—New Insights After More Than 75 Years of Clinical Use. Emerging Infectious Diseases, 12(2), 289–292.
- Hodgkin, D. (1965). Antibiotics. Scientific American, 212(2), 27–35.
- Hodgkin, D. (1969). Antibiotics: A Niche in Time. Proceedings of the Royal Society of Medicine, 62(1), 14–17.
- Ligon, B. L. (2004). Penicillin: Its Discovery and Early Development. Seminars in Pediatric Infectious Diseases, 15(1), 52–57.
- Lax, E. (2004). Antibiotics: From Prehistory to the Present Day. The Yale Journal of Biology and Medicine, 77(4), 205–215.
- Mahoney, J. C., & Ebert, M. C. (2011). Penicillin: A Paradigm for Biomedical Discovery. Yale Journal of Biology and Medicine, 84(3), 261–270.
- Podolsky, S. H. (2005). Antibiotics in American History. Issues in Science and Technology, 21(2), 61–66.
- Rees, A. R. (2001). Dorothy Hodgkin (1910–1994). Nature Structural Biology, 8(2), 93–94.
- Saad, R., & Morrison, S. S. (2020). Alexander Fleming (1881–1955): Discoverer of Penicillin. American Journal of Public Health, 110(11), 1627–1628.
- Wainwright, M. (1995). Alexander Fleming and the Development of Penicillin. Pediatric Infectious Disease Journal, 14(8), 705–707.
- Waksman, S. A. (1964). Search for Antibiotics: Fifty Years Later. Journal of Industrial Microbiology, 13(2), 119–123.