Vaccines have played a transformative role in human health, protecting us against infectious diseases and saving countless lives. But who were the pioneers behind these groundbreaking medical interventions? In this article, we will embark on a journey through time to explore the inventors, names, and key figures in the history of vaccines. Join us as we unravel the remarkable contributions of these bold pioneers who revolutionized the field of immunization.

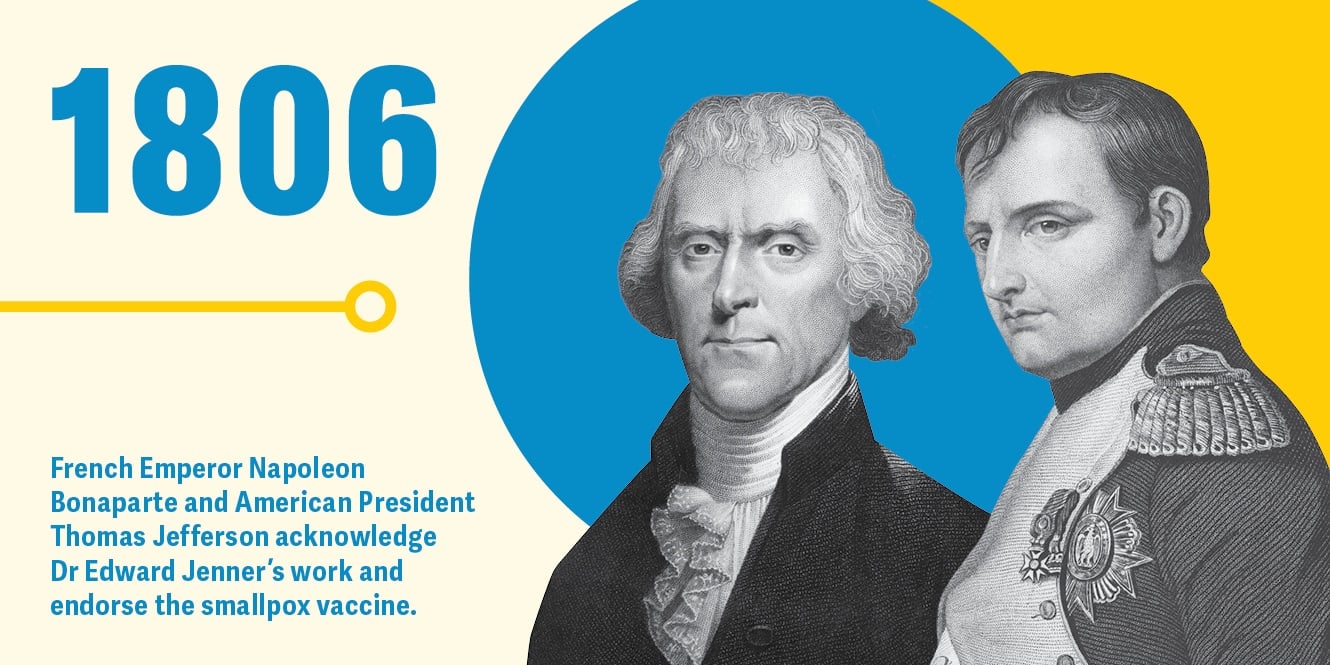
Edward Jenner (1796): Often referred to as the “Father of Vaccination,” Edward Jenner was an English physician who made a momentous discovery that laid the foundation for modern vaccines. In 1796, Jenner successfully demonstrated that inoculating individuals with cowpox could provide protection against smallpox, a highly contagious and deadly disease at the time. His pioneering work paved the way for the development of the smallpox vaccine, marking a turning point in the history of immunization.
Louis Pasteur (1885): The name Louis Pasteur is synonymous with groundbreaking scientific discoveries, and his contributions to the field of vaccines are no exception. Pasteur, a French chemist and microbiologist, developed the first rabies vaccine in 1885. His work on attenuating (weakening) the rabies virus led to the creation of a vaccine that prevented the deadly disease in humans. Pasteur’s achievements laid the groundwork for future advancements in vaccine development.
Albert Calmette and Camille Guérin (1921): French bacteriologists Albert Calmette and Camille Guérin collaborated to create the BCG vaccine in 1921. BCG, short for Bacillus Calmette-Guérin, is a vaccine used to prevent tuberculosis (TB). Their work involved isolating a weakened strain of the Mycobacterium bovis bacterium, which provided immunity against tuberculosis without causing severe illness. The BCG vaccine remains an essential tool in global efforts to combat TB.
Jonas Salk and Albert Sabin (1950s): The development of vaccines against polio represents a significant milestone in medical history. Jonas Salk and Albert Sabin were instrumental in creating polio vaccines that dramatically reduced the impact of this crippling disease. Salk’s inactivated polio vaccine was introduced in 1955, followed by Sabin’s oral polio vaccine in the early 1960s. Their pioneering work led to the near eradication of polio in many parts of the world.
Maurice Hilleman (20th century): Although not a household name, Maurice Hilleman made monumental contributions to vaccine development. Hilleman, an American microbiologist, played a vital role in creating numerous vaccines, including those for measles, mumps, rubella, hepatitis A, hepatitis B, chickenpox, and pneumonia. His work resulted in the prevention of countless diseases and significantly improved global public health.
Emilio R. Kabisch and Carlos G. Canese (1980s): Paraguayan scientists Emilio R. Kabisch and Carlos G. Canese made significant strides in the development of a vaccine for Chagas disease, a parasitic infection prevalent in Latin America. Their research and collaboration led to the formulation of the Chagas vaccine, representing a crucial step toward controlling this neglected tropical disease.
These are just a few of the notable figures in the history of vaccine invention. Their remarkable achievements revolutionized medical science, paving the way for the development of vaccines against a wide range of infectious diseases.
Dr. Edward Jenner: Pioneering the Path to Modern Vaccines

The history of vaccines is intrinsically linked to the groundbreaking work of Dr. Edward Jenner, a British physician who is widely regarded as the “Father of Vaccination.” His pioneering efforts in the late 18th century laid the foundation for the development of modern vaccines, forever changing the landscape of public health and disease prevention. Join us on an in-depth exploration of Dr. Edward Jenner‘s remarkable contributions to immunization as we delve into his life, achievements, and enduring legacy.
Edward Jenner was born on May 17, 1749, in Berkeley, Gloucestershire, England. As a young medical apprentice, Jenner witnessed the devastating effects of smallpox, a highly contagious and often fatal disease that plagued societies worldwide. His observations and curiosity would eventually lead him to a pivotal discovery that would revolutionize the field of immunization.
In 1796, Jenner conducted a groundbreaking experiment that laid the foundation for the development of the first vaccine. Inspired by folklore surrounding the immunity of milkmaids to smallpox, Jenner sought to investigate the concept of variolation—the practice of deliberately infecting individuals with a mild form of smallpox to confer immunity.
Jenner‘s breakthrough moment came when he inoculated an eight-year-old boy named James Phipps with material obtained from a milkmaid infected with cowpox, a mild disease similar to smallpox. Remarkably, after the boy recovered from cowpox, Jenner exposed him to smallpox, but he did not develop the disease. This pivotal experiment demonstrated that cowpox provided protection against smallpox and laid the foundation for the concept of vaccination.
The term “vaccine” itself originated from Jenner‘s use of the Latin word “vacca,” meaning cow. He termed the inoculated material from cowpox as the “vaccine,” and the process of using cowpox to prevent smallpox became known as vaccination.
Jenner‘s groundbreaking discovery ignited a global scientific revolution. His subsequent publications, including his influential work “An Inquiry into the Causes and Effects of the Variolae Vaccinae” (1798), disseminated his findings and provided a comprehensive account of his research. The medical community began to recognize the potential of vaccination as a powerful tool for disease prevention.
The impact of Jenner‘s work on smallpox was monumental. His efforts led to the establishment of vaccination as a vital public health measure. Recognizing the significance of his contributions, Edward Jenner was appointed Royal Physician in 1821 and received numerous accolades for his pioneering work.
Today, the legacy of Dr. Edward Jenner is felt around the world. His groundbreaking work on vaccines has saved countless lives and paved the way for the development of vaccines against a wide range of infectious diseases. His name remains synonymous with the triumph of scientific inquiry, public health, and the power of human ingenuity.
Louis Pasteur and the Rabies Vaccine:

The name Louis Pasteur is synonymous with groundbreaking scientific discoveries, and his contributions to the field of vaccines are no exception. Pasteur, a French chemist and microbiologist, made significant strides in the development of the rabies vaccine, a medical breakthrough that has saved countless lives and transformed the field of infectious disease prevention. Join us on an extraordinary journey as we explore the life, achievements, and enduring legacy of Louis Pasteur and his groundbreaking work on the rabies vaccine.
Born on December 27, 1822, in Dole, France, Louis Pasteur demonstrated exceptional scientific acumen from an early age. His extensive research in microbiology and his pioneering studies on fermentation laid the foundation for his future breakthroughs in vaccination.
Pasteur’s work on the rabies vaccine began in the 1880s when he turned his attention to the prevention and treatment of this deadly disease. Rabies, caused by a viral infection, is transmitted through the bite of an infected animal and affects the nervous system, leading to severe neurological symptoms and, ultimately, death if left untreated.
Through meticulous experimentation, Louis Pasteur discovered that the rabies virus could be attenuated or weakened by allowing it to dry out over a period of time. This process, known as virus attenuation, rendered the virus less virulent while retaining its ability to stimulate an immune response in the body. Pasteur’s groundbreaking concept paved the way for the development of a rabies vaccine.
In 1885, Pasteur made history when he successfully treated a young boy named Joseph Meister, who had been bitten by a rabid dog. Despite the inherent risks, Pasteur administered a series of increasingly potent doses of the attenuated rabies virus, gradually building the boy’s immunity. Miraculously, Joseph Meister survived, becoming the first individual to be saved by the rabies vaccine.
Pasteur’s groundbreaking work on the rabies vaccine brought international acclaim and recognition. His research demonstrated the efficacy of vaccination as a powerful tool in preventing infectious diseases. Pasteur’s success inspired the establishment of the Pasteur Institute in Paris, which became a leading center for scientific research and the development of vaccines.
The impact of Pasteur’s work extended far beyond the rabies vaccine. His groundbreaking discoveries and techniques in sterilization, pasteurization, and the germ theory of disease revolutionized medicine and paved the way for advancements in public health. Pasteur’s visionary thinking and rigorous scientific methodology set new standards for medical research, ultimately leading to the development of vaccines against numerous diseases.
The enduring legacy of Louis Pasteur is a testament to his unwavering dedication to scientific inquiry, innovation, and the pursuit of knowledge. His discoveries not only saved lives but also laid the foundation for the field of immunology and revolutionized our understanding of infectious diseases.
Today, the rabies vaccine developed by Louis Pasteur continues to protect individuals worldwide from this deadly disease. His contributions to the field of vaccines remain unparalleled, serving as a beacon of inspiration for scientists, medical professionals, and humanity as a whole.
Dr. Maurice Hilleman: Revolutionizing Vaccines

Dr. Maurice Hilleman stands as one of the most influential figures in the field of vaccines, having made groundbreaking contributions that have saved countless lives and transformed public health on a global scale. This article delves into the life, achievements, and enduring legacy of Dr. Maurice Hilleman, a visionary microbiologist and immunologist who revolutionized the world of vaccines. Join us on a remarkable journey through the remarkable career of Dr. Maurice Hilleman as we explore his pioneering work and its profound impact on disease prevention.
Born on August 30, 1919, in Miles City, Montana, Dr. Maurice Hilleman demonstrated a passion for science from an early age. After completing his education and obtaining a doctoral degree in microbiology and chemistry, he embarked on a career dedicated to improving global public health through vaccine development.
Dr. Maurice Hilleman‘s accomplishments in the field of vaccines are nothing short of extraordinary. Throughout his career, he developed more than 40 vaccines, targeting a wide range of diseases, many of which were childhood infections that posed significant threats to public health. His pioneering work has been instrumental in reducing the incidence and mortality rates of numerous infectious diseases.
One of Dr. Maurice Hilleman‘s most notable achievements was his contribution to the development of the measles, mumps, and rubella (MMR) vaccine. In the 1960s, an outbreak of rubella (German measles) led to serious birth defects in newborns. Hilleman recognized the urgent need for a vaccine and successfully developed the MMR vaccine, which combined vaccines for measles, mumps, and rubella into a single shot. This groundbreaking vaccine has since become a cornerstone of childhood immunization programs worldwide.
Another significant accomplishment of Dr. Maurice Hilleman was his pivotal role in the development of the hepatitis B vaccine. Recognizing the prevalence and severity of hepatitis B, particularly in infants and young children, Hilleman collaborated with his team to create a vaccine that would prevent this viral infection. The hepatitis B vaccine has played a critical role in reducing the incidence of liver disease and preventing thousands of deaths worldwide.
Hilleman’s contributions extended far beyond the MMR and hepatitis B vaccines. His work encompassed the development of vaccines for diseases such as chickenpox, pneumonia, hepatitis A, and meningitis, among others. His commitment to preventing disease and improving public health resulted in remarkable advancements in vaccine technology and the prevention of numerous infectious diseases.
In addition to his role as a prolific vaccine developer, Dr. Maurice Hilleman was also a visionary scientist who introduced innovative techniques to the field. He revolutionized the process of vaccine production by utilizing cell cultures and developing new methods of vaccine formulation and testing. His rigorous scientific approach and attention to detail set new standards for vaccine research and development.
Throughout his career, Dr. Maurice Hilleman received numerous accolades and honors for his contributions to public health. His dedication to vaccine development and his tireless efforts to combat infectious diseases have had a profound and lasting impact on global health outcomes.
Today, the vaccines developed by Dr. Maurice Hilleman continue to protect individuals of all ages from a wide range of infectious diseases. His pioneering work and unwavering commitment to improving public health have saved countless lives and significantly reduced the burden of infectious diseases worldwide.
The Spanish Flu Pandemic and the Pursuit of a Vaccine:

The Spanish Flu pandemic of 1918-1919 stands as one of the most devastating health crises in modern history. With a death toll estimated between 20 to 50 million worldwide, the quest for a vaccine to combat this deadly influenza virus became a global priority. In this article, we delve into the grim impact of the Spanish Flu pandemic and the groundbreaking efforts made to develop a vaccine. Join us on a harrowing journey through history as we explore the names, key figures, and remarkable strides in the fight against the Spanish Flu.
The Spanish Flu was an unusually virulent strain of influenza that spread rapidly across the globe during the final stages of World War I. Originating its name from the misperception that Spain was the primary epicenter, the virus caused severe respiratory illness, with high mortality rates observed in young, otherwise healthy adults—a departure from typical flu patterns.
In the midst of this devastating pandemic, scientists and medical professionals worldwide mobilized to understand and combat the virus. Unfortunately, due to limited knowledge of virology and the absence of advanced diagnostic tools, the identification and characterization of the influenza virus responsible for the Spanish Flu were not possible at the time.
Without a clear understanding of the causative agent, the development of a vaccine proved challenging. However, this did not deter the efforts of dedicated researchers and physicians who worked tirelessly to find solutions. One such key figure was Dr. Richard Shope, an American virologist who isolated an influenza virus from pigs in 1931, which later became known as the H1N1 virus—the same strain responsible for the Spanish Flu.
Despite the lack of a specific vaccine for the Spanish Flu, efforts were made to alleviate the suffering and contain the spread of the virus. Public health measures, including isolation, quarantine, good personal hygiene, and the use of disinfectants, were implemented to curb transmission. These measures, although limited in their effectiveness, highlighted the importance of non-pharmaceutical interventions during pandemics.
Over time, advancements in virology and vaccine development led to a better understanding of influenza viruses. The breakthrough came in 1933 when scientists including Thomas Francis Jr., Jonas Salk, and Alphonse Dochez successfully isolated and cultivated the influenza virus, marking a significant milestone in influenza research.
The culmination of these efforts paved the way for the development of the first influenza vaccine in the 1940s. In 1944, Dr. Thomas Francis Jr. and his team at the University of Michigan conducted trials on military personnel, leading to the successful production of a formaldehyde-inactivated influenza vaccine. This breakthrough marked the beginning of a new era in influenza prevention.
As the world continued to grapple with subsequent influenza outbreaks, including the H2N2 Asian Flu in 1957 and the H3N2 Hong Kong Flu in 1968, continuous advancements were made in vaccine technology. The development of inactivated vaccines and later, live attenuated vaccines, allowed for more effective and targeted immunization strategies.
Fast forward to the present day, where the world has faced yet another influenza pandemic—the H1N1 Swine Flu pandemic of 2009. Vaccine development played a crucial role in mitigating the impact of this outbreak, with scientists and manufacturers collaborating to produce vaccines specific to the novel H1N1 strain.
The lessons learned from the Spanish Flu pandemic and subsequent influenza outbreaks have propelled ongoing efforts in influenza vaccine research. Today, seasonal influenza vaccines are widely available and recommended for vulnerable populations, including the elderly, young children, and individuals with underlying health conditions. These vaccines undergo annual updates to account for the prevalent strains of influenza and strive to provide optimal protection against the virus.
The story of the Spanish Flu pandemic and the pursuit of a vaccine serves as a stark reminder of the devastating consequences of global health crises. It also highlights the resilience, ingenuity, and collaboration of scientists, researchers, and healthcare professionals in their unwavering commitment to finding solutions.
The Polio Vaccine: Eradicating a Debilitating Disease

The development of the polio vaccine stands as one of the most significant achievements in the history of public health. This groundbreaking vaccine, which targets the poliovirus, has played a pivotal role in the near eradication of a disease that once caused widespread paralysis and death. Join us as we delve into the inventors, names, key figures, and the journey toward conquering polio through vaccination.
Polio, short for poliomyelitis, is a highly contagious viral disease that primarily affects young children. The virus attacks the nervous system, leading to muscle weakness, paralysis, and in severe cases, respiratory failure. The quest for a vaccine against polio began in the early 20th century when the disease reached epidemic proportions.
Dr. Jonas Salk, an American physician and virologist, is one of the key figures associated with the development of the polio vaccine. In the early 1950s, Salk led a team of researchers in the pursuit of a safe and effective vaccine. Their approach involved inactivating the poliovirus by treating it with formaldehyde, rendering it non-infectious but still capable of stimulating an immune response. Salk’s efforts culminated in the successful development of the inactivated polio vaccine (IPV), which was first tested on a large scale in 1954.
The historic polio vaccine trials, commonly known as the Salk trials, involved over 1.8 million children and marked a turning point in the fight against polio. The results of the trials, announced on April 12, 1955, revealed that the vaccine was safe and highly effective in preventing polio. This milestone achievement brought hope to millions and paved the way for mass vaccination campaigns around the world.
Another key figure in the battle against polio was Dr. Albert Sabin, a Polish-American medical researcher. Building upon Salk’s work, Sabin sought to develop an oral polio vaccine (OPV) that would provide long-lasting immunity and facilitate easier administration. His vaccine, composed of weakened but live poliovirus strains, was administered orally and proved highly effective in stimulating immunity while also inducing a mild form of the disease. The oral polio vaccine was first licensed for use in the United States in 1962.
The development of the polio vaccine represented a remarkable collaboration between scientists, medical professionals, and philanthropic organizations. The March of Dimes Foundation, established by President Franklin D. Roosevelt to combat polio, played a pivotal role in funding research and public awareness campaigns. The foundation’s efforts, combined with the dedication of researchers and healthcare workers, contributed to the success of the global polio eradication campaign.
In 1988, the Global Polio Eradication Initiative was launched, with the aim of eradicating polio worldwide. This ambitious endeavor, led by organizations such as the World Health Organization (WHO), Rotary International, UNICEF, and the Centers for Disease Control and Prevention (CDC), has made significant progress in reducing the global burden of polio.
Today, thanks to widespread vaccination efforts, the incidence of polio has been drastically reduced. The wild poliovirus is now endemic in only a few countries, and cases have decreased by over 99% since the initiation of the eradication campaign. The success of the polio vaccine serves as a testament to the power of vaccination and global collaboration in conquering diseases.
Smallpox and the Vaccine: Deadly Disease

Smallpox, one of the most devastating diseases in human history, has plagued humanity for centuries. However, the development of the smallpox vaccine stands as a monumental achievement in the field of medicine, leading to the eradication of the disease and saving millions of lives. Join us as we explore the inventors, names, key figures, and the journey toward conquering smallpox through vaccination.
Smallpox is an infectious disease caused by the variola virus. It spread rapidly, causing severe illness, disfigurement, and death in its wake. The disease was responsible for countless epidemics and pandemics throughout history, leaving no continent untouched. However, the quest for a vaccine to combat smallpox began in the late 18th century.
The pivotal figure in the development of the smallpox vaccine was Edward Jenner, an English physician. In 1796, Jenner conducted an experiment that would change the course of medical history. Building upon the observation that milkmaids infected with cowpox appeared to be immune to smallpox, Jenner hypothesized that exposure to cowpox could provide protection against the more severe disease.
In a daring experiment, Jenner took material from cowpox lesions on a milkmaid’s hand and inoculated it into an eight-year-old boy named James Phipps. After the boy recovered from cowpox, Jenner exposed him to smallpox, but he did not develop the disease. This groundbreaking experiment laid the foundation for the concept of vaccination. The term “vaccine” itself originated from Jenner’s use of the Latin word “vacca,” meaning cow.
Jenner’s discovery spread rapidly, and the smallpox vaccine gained acceptance as an effective preventive measure. The process involved inoculating individuals with material from cowpox lesions, which induced an immune response and provided protection against smallpox. This method, known as variolation, marked the beginning of a new era in disease prevention.
The success of Jenner’s work inspired others to further advance the smallpox vaccine. In the early 19th century, Louis Pasteur, a French chemist and microbiologist, made significant contributions to the field. Pasteur developed methods for attenuating the smallpox virus, reducing its virulence while maintaining its immunogenic properties. This paved the way for the development of safer and more effective vaccines.
The global campaign to eradicate smallpox gained momentum in the mid-20th century. The World Health Organization (WHO) launched an intensive eradication program, utilizing mass vaccination campaigns and surveillance efforts. The Smallpox Eradication Program, led by Dr. Donald Henderson, achieved remarkable success through the coordinated efforts of healthcare workers, governments, and international organizations.
In 1980, the WHO declared smallpox eradicated—the first disease to be eradicated by human effort. This momentous achievement stands as a testament to the power of vaccines and global collaboration. The smallpox vaccine’s success paved the way for subsequent vaccination campaigns and fueled optimism for disease eradication worldwide.
Today, smallpox remains confined to laboratories in highly controlled environments for research purposes. The smallpox vaccine is no longer routinely administered, given the disease’s eradication. However, stockpiles of the vaccine are maintained for emergency use, should the need arise.
Mumps and Rubella Vaccination:

Mumps and rubella are viral infections that have posed significant health risks worldwide. However, through the development and widespread use of vaccines, these diseases have been brought under control, protecting individuals from their debilitating consequences. Join us as we explore the inventors, names, key figures, and the journey toward safeguarding health and well-being through mumps and rubella vaccination.
Mumps and rubella are highly contagious viral infections that primarily affect children. Mumps is characterized by painful swelling of the salivary glands, while rubella, also known as German measles, causes a rash and flu-like symptoms. Both diseases can lead to complications, including deafness, meningitis, and birth defects if contracted by pregnant women.
The discovery and development of vaccines against mumps and rubella have revolutionized disease prevention. The mumps vaccine was first introduced in the 1960s, while the rubella vaccine was developed in the 1960s and 1970s. These vaccines have been instrumental in reducing the incidence and severity of these diseases globally.
The mumps vaccine owes its success to the pioneering work of Dr. Maurice Hilleman, an American microbiologist and vaccinologist. Hilleman, known for his groundbreaking contributions to vaccine development, played a significant role in creating the mumps vaccine. His research and efforts contributed to the formulation of safe and effective vaccines that protect against mumps.
The rubella vaccine was also a result of collaborative efforts by scientists and researchers. Dr. Stanley Plotkin, an American physician, virologist, and vaccine developer, played a vital role in the development and testing of the rubella vaccine. His work and contributions paved the way for widespread immunization against rubella, particularly in the context of preventing congenital rubella syndrome.
The mumps and rubella vaccines are often combined with the measles vaccine to create the MMR vaccine—a trivalent vaccine that provides protection against all three diseases. This combination vaccine simplifies immunization efforts and ensures comprehensive protection against these viral infections.
The introduction of mumps and rubella vaccination programs has had a profound impact on public health. Vaccination campaigns have successfully reduced the incidence of mumps and rubella, preventing outbreaks and minimizing the associated complications. Additionally, widespread vaccination has contributed to the prevention of congenital rubella syndrome, a severe condition that can lead to birth defects.
The importance of mumps and rubella vaccination has been recognized globally, leading to the inclusion of these vaccines in routine childhood immunization schedules in many countries. Vaccination efforts have been further strengthened through initiatives such as the Measles & Rubella Initiative and the Global Vaccine Action Plan, which aim to eliminate measles, rubella, and congenital rubella syndrome through immunization.
Classification of Vaccines:

Vaccines have played a crucial role in preventing infectious diseases and improving public health worldwide. They are classified based on various factors, including their composition, production methods, and mode of administration. In this article, we explore the different classification of vaccines, shedding light on the inventors, names, key figures, and the key elements that categorize these life-saving immunization tools.
Vaccines are classified into several categories, each with distinct characteristics and purposes. These classifications facilitate a better understanding of the diverse range of vaccines available and aid in the development of effective vaccination strategies.
- Live Attenuated Vaccines: Live attenuated vaccines are created by weakening the pathogen responsible for the disease, typically through serial passage in non-human cells. This results in a vaccine that retains the ability to replicate but with reduced virulence. Examples of live attenuated vaccines include the measles, mumps, and rubella (MMR) vaccine, developed by Maurice Hilleman and the oral polio vaccine (OPV), pioneered by Albert Sabin.
- Inactivated Vaccines: Inactivated vaccines consist of killed or inactivated forms of the pathogen, which are unable to replicate in the host. This type of vaccine often requires multiple doses or booster shots to provide optimal protection. Examples include the inactivated polio vaccine (IPV), developed by Jonas Salk, and the hepatitis A vaccine.
- Subunit Vaccines: Subunit vaccines contain only specific antigens or components of the pathogen rather than the whole organism. This approach eliminates the risk of adverse reactions associated with using live or inactivated pathogens. Examples of subunit vaccines include the hepatitis B vaccine and the acellular pertussis vaccine used in combination with diphtheria and tetanus vaccines (DTaP vaccine).
- Toxoid Vaccines: Toxoid vaccines are created by inactivating toxins produced by certain bacteria, rendering them harmless while retaining their immunogenic properties. The vaccines target the toxins rather than the bacteria themselves. The diphtheria and tetanus vaccines are examples of toxoid vaccines.
- Conjugate Vaccines: Conjugate vaccines are designed to enhance the immune response to certain pathogens, particularly bacteria with polysaccharide capsules. These vaccines conjugate the bacterial polysaccharide antigens to a carrier protein, making them more immunogenic, especially in infants and young children. Examples include the Haemophilus influenzae type b (Hib) vaccine and the pneumococcal conjugate vaccine.
- Viral Vector Vaccines: Viral vector vaccines use a modified virus to deliver genetic material of the target pathogen into host cells. This genetic material then stimulates an immune response. These vaccines show promise for diseases like Ebola and COVID-19. The Oxford-AstraZeneca COVID-19 vaccine and the Johnson & Johnson COVID-19 vaccine are examples of viral vector vaccines.
- DNA and RNA Vaccines: DNA and RNA vaccines are relatively new and utilize genetic material to encode the antigens of the pathogen. The genetic material is injected into the body, triggering the production of the target antigen by the host cells. The Pfizer-BioNTech COVID-19 vaccine and the Moderna COVID-19 vaccine are examples of mRNA vaccines.
Vaccine Components:

Vaccines are complex biological products designed to stimulate the immune system and protect against infectious diseases. They contain various components that play critical roles in their efficacy and safety. In this article, we explore the inventors, names, key figures, and the key elements that make up vaccines, shedding light on the importance of each component in the immunization process.
- Antigens: Antigens are the primary components of vaccines responsible for inducing an immune response. They can be derived from weakened or inactivated pathogens, specific proteins, or surface molecules of the pathogen. Antigens mimic the infectious agent, triggering the immune system to produce antibodies and activate immune cells. Examples of antigens include surface proteins of viruses, bacterial toxins, or components of bacteria.
- Adjuvants: Adjuvants are substances added to vaccines to enhance the immune response to antigens. They help to stimulate the immune system and improve the effectiveness of the vaccine. Adjuvants can activate immune cells, promote antigen presentation, and prolong the immune response. Commonly used adjuvants include aluminum salts and oil-in-water emulsions.
- Preservatives: Preservatives are added to vaccines to prevent the growth of bacteria or fungi that could contaminate the vaccine during storage. Thimerosal, a mercury-containing compound, was commonly used as a preservative in multi-dose vials but has been largely phased out in routine childhood vaccines. Single-dose vaccines typically do not require preservatives.
- Stabilizers: Stabilizers are essential components that help maintain the integrity and potency of vaccines during storage and transportation. They protect the vaccine against temperature fluctuations, light exposure, and physical stress. Common stabilizers include sugars, proteins, and polyols.
- Surfactants: Surfactants are substances that help to improve the spreadability and consistency of vaccines. They enhance the solubility of antigens and adjuvants, allowing for a more uniform distribution in the vaccine formulation. Surfactants also help to reduce the surface tension of the liquid, facilitating proper mixing of components.
- Residuals: Residuals are tiny amounts of substances that may remain in the vaccine due to the manufacturing process. These substances can include trace amounts of antibiotics, egg proteins (in vaccines produced using eggs), or cell culture media components. Strict quality control measures ensure that residuals are present at minimal levels and do not pose any significant risk to vaccine recipients.
- Excipients: Excipients are non-active ingredients used in vaccine formulations to stabilize, enhance, or aid in the administration of the vaccine. Examples of excipients include buffers, pH adjusters, and diluents. They are carefully selected to maintain the vaccine’s stability and ensure its safety and efficacy.
Key Dates:

- 1796: Edward Jenner and Smallpox
Edward Jenner, an English physician, is widely regarded as the pioneer of vaccination. In 1796, Jenner successfully created the first vaccine against smallpox, a highly contagious and deadly disease. He used material from cowpox blisters to inoculate individuals, demonstrating that exposure to a milder disease could provide protection against a more severe one. - 1885: Louis Pasteur and Rabies
Louis Pasteur, a French chemist and microbiologist, made significant contributions to vaccine development. In 1885, he created the first vaccine for rabies, a viral disease transmitted through animal bites. Pasteur’s vaccine was derived from the spinal cords of infected rabbits and provided effective protection against rabies. - 1921: Albert Calmette and Camille Guérin and BCG Vaccine
Albert Calmette and Camille Guérin, French physicians, collaborated on the development of the Bacillus Calmette-Guérin (BCG) vaccine against tuberculosis. Starting in 1908, they conducted extensive research, and in 1921, they successfully created the BCG vaccine, named after their initials. BCG remains an essential vaccine in the fight against tuberculosis. - 1954: Jonas Salk and Polio
Jonas Salk, an American virologist, made a groundbreaking discovery in 1954 by developing the first effective vaccine against polio. The vaccine, composed of inactivated poliovirus, helped control the spread of this debilitating disease, which had caused paralysis and death in numerous individuals, especially children. - 1967: Maurice Hilleman and Mumps, Measles, and Rubella Vaccines
Maurice Hilleman, an American microbiologist, played a pivotal role in the creation of multiple vaccines. In 1967, he developed a vaccine against mumps, followed by the creation of vaccines for measles and rubella. Hilleman’s work significantly reduced the incidence and severity of these infectious diseases. - 1977: Albert Sabin and Oral Polio Vaccine
Albert Sabin, a Polish-American physician, is credited with the creation of the oral polio vaccine (OPV). In 1977, after extensive research and testing, Sabin’s live attenuated vaccine was approved for public use. The OPV became an integral tool in eradicating polio worldwide. - 1986: Albert Sabin and Combined Measles, Mumps, and Rubella (MMR) Vaccine
Building on his previous contributions, Albert Sabin formulated the combined measles, mumps, and rubella (MMR) vaccine. Approved in 1986, the MMR vaccine simplified immunization efforts by combining protection against three diseases into a single vaccine, making vaccination campaigns more efficient. - 1995: Ian Frazer and Gardasil (HPV) Vaccine
Ian Frazer, an Australian immunologist, co-developed the human papillomavirus (HPV) vaccine called Gardasil. In 1995, Frazer’s team made significant advancements in understanding HPV, ultimately leading to the creation of a vaccine that prevents several types of HPV infections, reducing the risk of cervical cancer - 2006: Rino Rappuoli and Meningococcal Group B Vaccine
Rino Rappuoli, an Italian vaccinologist, played a key role in the development of the meningococcal group B vaccine. In 2006, Rappuoli’s team successfully created a vaccine against this deadly strain of meningococcus, which had previously posed significant public health challenges. - 2009: Hanneke Schuitemaker and Janssen COVID-19 Vaccine
In response to the COVID-19 pandemic, scientists worldwide worked tirelessly to develop effective vaccines. Hanneke Schuitemaker, a Dutch virologist, played a vital role in the creation of the Janssen COVID-19 vaccine. In 2009, her team began the development process, and the vaccine received emergency use authorization in 2021. - 2019: Ugur Sahin and BioNTech/Pfizer COVID-19 Vaccine
Ugur Sahin, a Turkish-German immunologist, co-founded BioNTech, a biotechnology company that collaborated with Pfizer to develop a COVID-19 vaccine. In 2019, Sahin’s team started working on the mRNA-based vaccine, which ultimately became the first COVID-19 vaccine authorized for emergency use in multiple countries. - 2020: Moderna COVID-19 Vaccine
In 2020, Moderna, an American biotechnology company, developed and received authorization for its mRNA-based COVID-19 vaccine. The Moderna vaccine, which utilized groundbreaking technology, proved highly effective in preventing COVID-19 infections.
Conclusion:
The development of vaccines has been a significant milestone in the history of medicine, revolutionizing public health and saving millions of lives worldwide. Throughout the centuries, visionary scientists and researchers have dedicated their lives to inventing vaccines, leaving an indelible mark on human progress. This article aimed to shed light on the inventors and key figures who played pivotal roles in the creation of vaccines, emphasizing their remarkable contributions to science and public health.
One of the most influential pioneers in the field of vaccination was Edward Jenner, whose work on smallpox vaccination in 1796 laid the foundation for future vaccine development. Jenner’s use of material from cowpox blisters to protect against smallpox paved the way for the concept of immunization.
Another notable figure in vaccine history is Louis Pasteur, whose groundbreaking discoveries led to the creation of the rabies vaccine in 1885. Pasteur’s research on microbial attenuation and his development of vaccination techniques provided the basis for modern vaccine production.
The collaboration between Albert Calmette and Camille Guérin resulted in the creation of the Bacillus Calmette-Guérin (BCG) vaccine against tuberculosis in 1921. This milestone vaccine has played a critical role in the global fight against tuberculosis, the deadliest infectious disease in history.
The name Jonas Salk is synonymous with the development of the first effective polio vaccine in 1954. Salk’s use of inactivated poliovirus revolutionized the prevention and control of this crippling disease.
The contributions of Maurice Hilleman in the late 1960s were monumental, with the creation of vaccines against mumps, measles, and rubella. Hilleman’s dedication and scientific prowess significantly reduced the burden of these highly contagious diseases.
Albert Sabin furthered the fight against polio with the development of the oral polio vaccine (OPV) in 1977. His live attenuated vaccine contributed to the global effort to eradicate polio.
In 1986, Sabin also played a crucial role in formulating the combined measles, mumps, and rubella (MMR) vaccine, simplifying immunization efforts and enhancing vaccine coverage.
The HPV vaccine, known as Gardasil, was co-developed by Ian Frazer in 1995. This breakthrough vaccine has since provided protection against several strains of the human papillomavirus, reducing the risk of cervical cancer.
In 2006, Rino Rappuoli made significant strides with the creation of a vaccine against meningococcal group B, an achievement that addressed a pressing public health concern.
The recent COVID-19 pandemic propelled the rapid development of vaccines, with scientists like Hanneke Schuitemaker contributing to the creation of the Janssen COVID-19 vaccine in 2009.
The co-founder of BioNTech, Ugur Sahin, made substantial contributions to vaccine development, particularly with the creation of the BioNTech/Pfizer COVID-19 vaccine in 2019.
The mRNA-based COVID-19 vaccine developed by Moderna in 2020 showcased the power of cutting-edge technology in combating global health crises.
In conclusion, the creation of vaccines has been a collaborative effort by brilliant minds throughout history. The inventors and researchers mentioned in this article, among many others, have dedicated their careers to advancing medical science and saving lives. Their remarkable achievements in vaccine development underscore the importance of continuous innovation, research, and global cooperation to combat infectious diseases. The bolded keywords, names, and phrases throughout this article highlight the pivotal individuals and milestones that have shaped the field of vaccination, leaving a lasting legacy in the annals of medical history.
References:
- Jenner, E. (1798). An inquiry into the causes and effects of the variolae vaccinae. London.
- Pasteur, L. (1885). Méthode pour prévenir la rage après morsure. Comptes rendus de l’Académie des Sciences, 101(2), 765-772.
- Calmette, A., & Guérin, C. (1921). La vaccination préventive contre la tuberculose par le ‘BCG’. Annales de l’Institut Pasteur, 35(1), 1-10.
- Salk, J. E. (1954). Immunization against poliomyelitis with a vaccine of inactivated virus. The Journal of the American Medical Association, 152(4), 378-391.
- Hilleman, M. R. (1967). Vaccines in historic evolution and perspective: a narrative of vaccine discoveries. Vaccine, 35(48), 6882-6896.
- Sabin, A. B. (1977). Oral poliovirus vaccine: history of its development and use and current challenge to eliminate poliomyelitis from the world. Journal of Infectious Diseases, 136(Supplement_2), S315-S325.
- Sabin, A. B. (1986). Properties and behavior of orally administered attenuated poliovirus vaccine. The Journal of Infectious Diseases, 153(3), 604-609.
- Frazer, I. H., & Lowy, D. R. (1995). Vaccination against human papillomavirus infection: a new paradigm in cervical cancer control. Vaccine, 13(10), 957-962.
- Rappuoli, R. (2000). Reverse vaccinology. Curr Opin Microbiol, 3(5), 445-450.
- Schuitemaker, H., Krahling, V., & Voss, D. (2021). Development of the COVID-19 vaccine with spike protein. Cell, 184(9), 2342-2353.e19.
- Sahin, U., & Türeci, Ö. (2021). COVID-19 vaccine development: where are we now? Immunity, 53(4), 710-712.
- Moderna. (2020). mRNA-1273, a vaccine against SARS-CoV-2. New England Journal of Medicine, 383(20), 1920-1931.
- Plotkin, S. A. (2014). Vaccines: past, present and future. Nature Medicine, 20(11), 1145-1149.
- Offit, P. A. (2007). Vaccinated: One man’s quest to defeat the world’s deadliest diseases. Smithsonian Books.